When sinus symptoms linger long enough to feel like part of your daily routine, it can get frustrating and confusing. You try treatments, you wait for recovery, but the congestion, pressure, and discomfort keep coming back. This usually happens when a lesser-known cause, like a fungal sinus infection, is at the root of it.
These infections can closely resemble regular sinusitis, which is why they’re often overlooked. The only way to know for sure is through proper testing. Knowing when to get tested and which tests work best can help you get the right diagnosis for lasting relief.
In this guide, we’ll explore how fungal sinus infections are tested and what doctors look for before guiding you towards the right treatment option.
Table of Contents
ToggleWhat is a Fungal Sinus Infection?
A fungal sinus infection occurs when fungi (microorganisms found in the environment, such as air, soil, and plants) begin to grow within the sinus cavities. Most people naturally inhale fungal spores without any harm, as a healthy immune system can easily filter them out. The problem begins when the immune system isn’t strong enough to clear them effectively.
It also gets worse when the sinuses become warm, moist, and blocked, creating the perfect environment for them to thrive. This can lead to inflammation, congestion, and persistent sinus discomfort that doesn’t improve with standard treatments.
Difference Between Bacterial vs. Fungal Sinus Infections
Here’s a quick comparison to help you see the main differences between bacterial and fungal sinus infections.
| Feature | Bacterial Sinus Infection | Fungal Sinus Infection |
| Cause | Caused by bacteria entering the sinuses | Caused by fungi growing in the sinuses |
| Response to Treatment | Usually improves with antibiotics | Does not respond to antibiotics |
| Duration | Typically lasts a few days to weeks | Can be chronic or recurrent, lasting months |
| Mucus | Usually thin or yellow/green | Often thicker and darker |
| Symptoms | Nasal congestion, facial pressure, mild loss of smell | Increased facial pressure, reduced sense of smell, persistent congestion |
Why Fungal Cases Are Often Misdiagnosed
Fungal sinus infections can be tricky because they often look just like regular sinus infections. The usual signs of congestion, facial pressure, and nasal discharge are very similar to bacterial sinusitis, so many people are treated with antibiotics first. When symptoms don’t improve, it can take longer to realize a fungal infection is the real cause.
Adding to the challenge.
- Not all fungal infections cause severe symptoms, so they can be hard to spot early.
- Routine tests sometimes don’t detect fungi right away.
- Without specialized tools such as nasal endoscopy or lab tests, the infection can easily go unnoticed.
This is why proper evaluation is essential. Identifying the root cause early can help guide a more effective treatment plan.
When Should You Get Tested?
Not every sinus infection calls for detailed testing. However, if symptoms persist and treatments such as antibiotics, nasal sprays, or decongestants offer little to no relief, you should consider getting tested. Below are some key indicators you can keep an eye on.
- Symptoms last longer than 12 weeks, even with treatment.
- Sinus pressure or headaches become more intense over time.
- Your nasal discharge turns dark, unusually thick, or foul-smelling.
- You rely heavily on medications to manage daily discomfort.
- You notice symptoms worsen after being in damp, dusty, or mold-prone environments.
- Breathing feels restricted, or there’s a consistent blockage on one side of the nose.
Diagnostic Tests for Fungal Sinus Infection
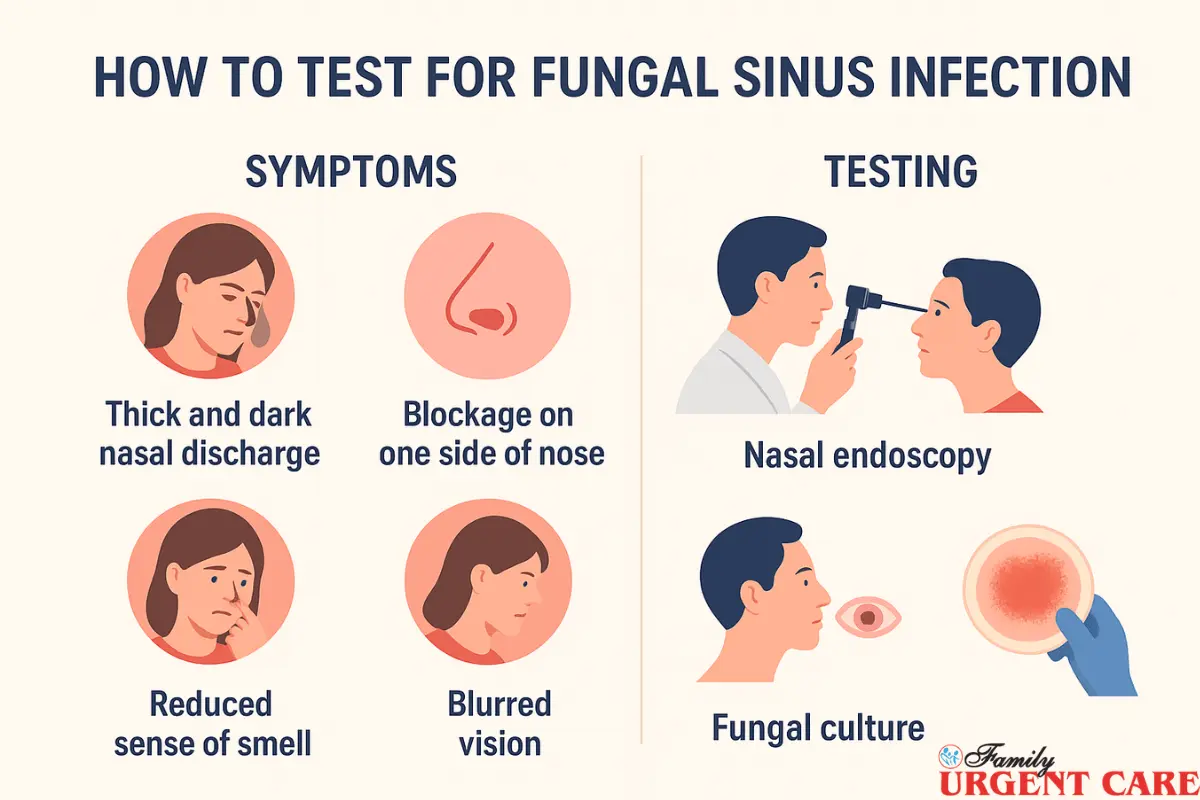
Diagnosing a fungal sinus infection involves a combination of clinical evaluation, imaging, and lab tests to pinpoint the cause. Early and accurate testing helps ensure the right treatment and faster relief. Here are some of the best ways doctors go about it.
Clinical Evaluation
The first step in diagnosing a fungal sinus infection is through a clinical evaluation. This helps your doctor understand your symptoms and decide which tests are needed.
Medical History & Symptoms Review
Your doctor will start by asking detailed questions about your symptoms like how long they’ve lasted, how severe they are, and what treatments you’ve tried so far. They may also ask about your environment, allergies, or any conditions that could weaken your immune system. This information helps identify if your sinus issues are due to fungi or bacteria.
Nasal Endoscopy
Nasal endoscopy is a simple procedure that allows your doctor to look directly into your nasal passages and sinuses. They use a small, flexible tube with a light and a camera. It’s usually quick and can be done in the clinic.
During this exam, the doctor can check for fungal debris, polyps, or areas of inflammation that may not be visible on regular scans. This step is often crucial for spotting fungal infections that would otherwise go unnoticed.
Imaging Tests
Imaging tests help doctors see inside your sinuses in ways that aren’t possible with a physical exam alone. They provide a clear picture of blockages, inflammation, and any potential fungal growth. This helps guide further testing or treatment with ease.
CT Scan
A CT scan is usually the first imaging test your doctor will use if a fungal sinus infection is suspected. It takes detailed pictures of your sinuses, showing any blockages, thickened tissue, or areas where fungal debris might be building up. CT scans are especially useful for planning treatment or surgery, as they clearly reveal the exact location and extent of the infection.
MRI
An MRI gives doctors a closer look at the soft parts of your sinuses and the areas around them. It helps detect small or hidden fungal infections, assess for complications, and identify inflammation that might not appear on a CT scan. Doctors usually use an MRI for persistent or tricky cases where they need a very clear picture before deciding on treatment.
Laboratory Tests
Laboratory tests play a crucial role in confirming a fungal sinus infection. They help doctors identify the exact type of fungus and determine the best treatment approach.
Fungal Culture & Microscopy
A fungal culture involves taking a small sample of nasal mucus or sinus tissue and growing it in a lab to detect the presence of fungi. Under a microscope, doctors can observe the fungal structures directly. It helps them confirm the infection and, sometimes, identify the specific type of fungus. This test is often one of the first steps when a fungal infection is suspected.
Tissue Biopsy
In some cases, doctors may recommend a tissue biopsy, where a small piece of sinus tissue is collected and examined in a lab. It is known as the most reliable method for diagnosing fungal sinus infections, as it can detect even hidden fungal growth that other tests might miss. A biopsy also helps determine the severity and type of infection. This guides towards the most effective treatment option possible.
Blood Tests
Blood tests help doctors detect signs of allergies or inflammation in your body. If your IgE levels or eosinophil count are higher than normal, it may indicate that your immune system is reacting to a fungal infection. These tests don’t confirm a fungal infection on their own, but they give helpful clues and show how your body is responding.
Interpreting the Test Results
Once your doctor has reviewed the tests, the results help identify the type of fungal sinus infection and offer the right treatment approach.
Types of Fungal Sinus Infections
- Allergic Fungal Rhinosinusitis (AFRS): This type occurs when the body reacts to fungus in the sinuses with an allergic response. Symptoms are often chronic but non-invasive. This means that the fungus doesn’t spread into surrounding tissues.
- Acute Invasive Fungal Sinusitis: A rapidly progressing infection that can spread quickly into surrounding tissues. This type is rare but serious, often affecting people with weakened immune systems.
- Chronic Invasive Fungal Sinusitis: A slow-growing infection that may develop over months. It can gradually damage sinus tissue if not treated. This usually affects people with slightly weakened immune systems or other health issues.
What Your Results Mean for Treatment
Understanding the specific type of fungal sinus infection helps your doctor choose the most effective treatment. For instance,
- Allergic forms may be treated with corticosteroids to reduce inflammation and sometimes antifungal medication to limit fungal growth.
- Acute invasive infections require urgent medical attention. It often includes antifungal drugs and sometimes surgery to remove infected tissue.
- Chronic invasive infections may need long-term antifungal medication. Sometimes, minor surgery is also required to remove stubborn fungal material.
By interpreting the results, Doctors tailor the treatment to your condition. This helps relieve symptoms faster and prevent complications before they get worse.
Conclusion
Fungal sinus infections can be tricky, but early diagnosis and testing can keep them from taking over. If your sinus symptoms are worsening, visit Family Urgent Care at your earliest convenience. We offer a wide range of tests to identify the cause and accurately guide the right treatment.
Reach out today and take the first step toward healthier sinuses.
FAQs
Q 1: What are the signs that I might have a fungal sinus infection?
Watch for persistent congestion, facial pressure, thick or dark nasal discharge, loss of smell, or symptoms lasting more than 12 weeks. If your sinus issues don’t improve with usual treatments, it could be fungal.
Q 2: How do doctors test for a fungal sinus infection?
Testing usually starts with a clinical evaluation, during which your doctor reviews your symptoms and medical history. They may perform a nasal endoscopy to look inside your sinuses and detect any fungal buildup or inflammation.
Q 3: Do I need scans or lab tests to confirm it?
Often, yes. CT scans can detect blockages or fungal debris, while an MRI can provide a clearer view of soft tissues in complex cases. Lab tests, like fungal cultures, tissue biopsies, and blood tests, help confirm the infection and guide treatment.
Q 4: What happens after the tests?
Test results help your doctor determine the type of fungal sinus infection, such as an allergic, acute invasive, or chronic invasive infection. Knowing the type helps choose the suitable treatment. It may include medication, minor surgery, or both, depending on severity.


